UHC+MDT: A chain of thoughts
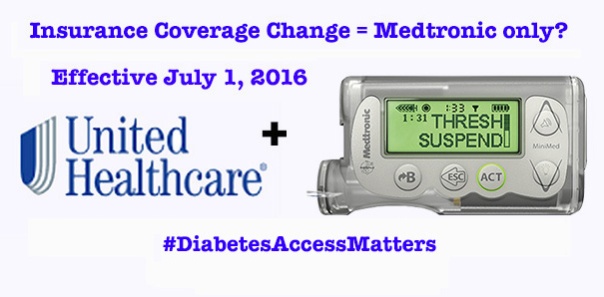
Image via DiabetesMine
I am, for the most part, not an emotional guy when it comes to diabetes. It’s something I’ve got and something I need to deal with. There’s no point in whining or complaining, because that doesn’t help.
Perhaps that’s why I’m so confused by the wave of emotions and thoughts that come to mind over the recent UHC/Medtronic development. Perhaps I don’t do well with emotion. Perhaps I don’t understand it.
This post is NOT going to be about how wrong that decision is, or how people deserve better, or anything like that. This post is going to be about everything that I’ve been thinking and feeling since hearing this news, and how I’ve tried to understand and make sense of it all. My hope is that, in writing it, I discover some clarity myself – and maybe I’ll impart some knowledge or thoughts along the way.
1. I’ve been betrayed.
Just a few weeks ago, I, along with many others, was an invited guest at Medtronic’s headquarters. Our hosts made a big point to show how they are shifting their focus to one that is patient-centric. The “bully” of pump companies was, in effect, becoming a kindler and gentler Medtronic.
While there, I established relationships with some of their staff and strengthened existing relationships with others. Now, I’m not sure where those relationships stand.
2. Maybe it makes sense. All pumps are, essentially, the same.
When it comes to treating people’s health, glitz and glamour doesn’t matter. The differences between various manufacturers’ pumps are not that great. Some have buttons; some have colors; some are touch-sensitive; some communicate directly with meters and/or CGMs so you don’t have to. But in the end, they all deliver insulin in more or less the same way. So, unless someone has particular needs (not the same as wants) for reasons such as vision impairment, high insulin needs, or very low-dose precision, does it really matter?
So, if we accept the thought that the differences between pumps are largely superficial, and that the exclusivity is purely price-driven, I ask…
3. Would I rather see 50% of PWDs be given affordable access to their choice of pump, or see 100% of PWDs be given access to a pump that is chosen for them?
The percentages are hypothetical and purely for the sake of discussion. But if this drives the price down to the point where everyone (under UHC coverage, for now) can get one, is it worth it? Being in the former 50% category today, I’m satisfied with the way things are. But that’s a rather selfish standpoint to take.
4. Should I even be angry? Though I am covered under UHC, I have freely chosen to use Medtronic for the past ten years, and all signs (prior to this week) point to me selecting Medtronic again.
I hate getting angry for the sake of getting angry. In many cases, there’s really no point in making a scene. This really doesn’t matter to me.
Although, it might. Who’s to say what innovations may come down the road from someone else? And though I just received a new Dexcom G4 transmitter (to replace the Dexcom G4 transmitter I got 6 months ago, both of which are sitting in a cabinet as the Dexcom G4 transmitter I got 6 months before that continues to chug along faithfully), this deal may very well extend to CGMs; then I will be affected. And speaking of CGM….
5. It was about this time last year when Medtronic finally “convinced” United Healthcare that the 530G with Threshold Suspend was indeed beyond “experimental” and should be covered. Coincidence?
I didn’t believe then that it was a matter of convincing, rather a matter of negotiating. And I certainly don’t believe it now. The terms of this agreement were put in place a year ago, right? I’ll bet UHC just needed to let the terms run out on its other contracted companies before they could go full-throttle with this one. Knowing – or even thinking – that this has been going on right under my nose makes me extremely resentful. It also helps to clarify….
6. Who should I be mad at? Is United Healthcare to blame? Is Medtronic to blame? Both?
Lots of folks have told me that Medtronic engaged in this deal simply as a business decision, to expand distribution of their product. They tell me that if Medtronic hadn’t negotiated prices low enough to be UHC’s exclusive supplier, then someone else would have. They tell me not to be mad at Medtronic.
Meanwhile, United Healthcare has been very good to me for a very long time. I’ve been under several different medical plans underwritten by several different employers since finishing college and going on my own medical plan, and every one of them has been administered by UHC. Considering all the gripes that people have had with insurers, I see UHC as one of the good ones.
But times change, and these backroom negotiations do happen – and they are sleazy. As for the people conducting these negotiations…
7. I’ve got friends in low places. I don’t want to hurt them.
A college buddy of mine works for United Healthcare. Through my activity in the DOC, I’ve gotten to know folks at Medtronic Diabetes on a first-name basis. I work hard to maintain these relationships, and try to build new ones.
The communications folks at MDT are in a really difficult place right now. I feel bad for the task they are up against. They didn’t cause this to happen, yet they are left to pick up the pieces. And in the midst of all of this unfolding, my UHC friend posted a rainy-day photo of his office – corporate logo on top – on Facebook.
And I exploded. I lashed out at Medtronic Diabetes and at UHC all over social media.
I feel really bad for the people on the other side of those lashes. I love those people; I really do. My moral conscience is torn between sticking up for my friends and sticking up for what’s right.
8. How can this be fixed?
Immediately, I knew that the Diabetes Community would be up in arms over this exclusivity. I knew that they would take to social media to voice their complaints (as I did). I also know that the Diabetes Community tends to get a bit noisy and obnoxious, and tends to raise hell over just about everything, and this would likely get dismissed.
What is the underlying premise that makes UHCs and MDTs actions so wrong? This is not about choice. This is not about diabetes. This is about insurers playing doctor, and choosing the best treatments based on financial, rather than medical knowledge. The problem extends well beyond insulin pumps and well beyond diabetes. Perhaps some folks in our community have relationships with other medical communities (via HealtheVoices, for instance) and can get some anecdotes.
The argument that needs to be made is this: insurers should not be allowed to dictate treatment. The argument needs to be made at a regulatory, governmental level.
Because there’s no way in hell the insurers are going to be shamed into fixing it themselves. I know this because…
9. United Healthcare is full of crap
In his Happy-Medium blog, Stephen dug up (I urge you to visit that site to read his thought) the “Mission Statement” of United Health Group, UHC’s parent company.
In United Health’s words:
“We seek to enhance the performance of the health system and improve the overall health and well-being of the people we serve and their communities.”
“We work with health care professionals and other key partners to expand access to quality health care so people get the care they need at an affordable price.”
“We support the physician/patient relationship and empower people with the information, guidance, and tools they need to make personal health choices and decisions.”
Or, to paraphrase (in my words):
We are the biggest bullshit artists around, and we’ll say whatever it takes to get people to like us, but when push comes to shove, we always win! MUAHAHAHA!
Now, I’m sure that someone at UHC will try to defend their actions, saying that the Affordable Care Act is causing them to lose tons of money and that sacrifices need to be made in order to keep afloat.
But this picture tells a very different story.

UHC’s stock price
10. We are all just guinea pigs in a sick, sick game
The truth (or what I perceive to be the truth) finally came to me as I was reading the Storify coverage of the event put together by DiabetesMine.
Particularly, it was this paragraph – a quote from a spokesperson, and (hopefully) still a friend at MDT, that made it click:
“In addition, our two companies will work together to help advance diabetes care and find new ways to analyze the total cost of care for diabetes management, including how advanced technologies and patient support can improve individuals’ care plans. We aspire to bring a value-based approach to diabetes care that tracks clinical outcomes for UnitedHealthcare members on insulin pumps and places greater focus on quality rather than the volume of care delivered.”
During the Diabetes Advocates Forum, there were some recurring themes that seemed odd in their ambiguity. The buzzwords were: Data. Partnerships. Better Diabetes Outcomes.
Data was a big thing – they’ve been talking a lot about data, and even hired a data-guru executive to lead the effort, but they were never clear on how it would be used. They were going to pull data from all over the place to reach all sorts of groundbreaking conclusions. One such conclusion, for which they already (apparently) had evidence, is that pumping is, overall, cheaper than MDI.
Now I see where they are going with this.
This is all speculation on my part, but if I’m putting the pieces together properly, it makes sense:
- In exchange for low-cost supplies to UNITED HEALTHCARE consumers, MEDTRONIC DIABETES is receiving data from UHC regarding how often we see doctors, purchase test strips, etc., and how much we pay for them.
- Using their Watson Supercomputer Thingamajig, MEDTRONIC DIABETES is aggregating the data they get from UHC with the data they get from pump-uploads via CareLink (which, if MiniMed Connect is any indication, will soon become automatic and possibly involuntary)
- From these CareLink reports, MEDTRONIC DIABETES can tell UNITED HEALTHCARE how often we actually use the supplies that they help us buy, so that they can prevent those who (allegedly) build up a stash from doing so
Essentially, Medtronic is developing a comprehensive medical profile on us. They’ll study how Threshold Suspend affects the number of times the ambulance is called. They’ll look at how often a patient receives (and submits a claim for) an A1C test, and how the frequency of A1C tests does or does not affect a patient’s blood sugars. They’ll look at the total costs of pumping, including supplies, prescriptions, and labwork, and compare them to UHC’s databases on those who don’t use pumps.
I’m not sure how far they will take this, or how far HIPAA will allow it. But it’s all becoming crystal clear to me.
This isn’t about saving money. This is about gathering subjects for a massive data research project.
Data that will, undoubtedly, somehow become monetized.
Perhaps the research will prove valuable. Perhaps not.
But I didn’t sign up for the study. I wasn’t recruited.
I was forced.
I deeply resent that.
Posted on May 5, 2016, in Diabetes. Bookmark the permalink. 22 Comments.

Very well put. I’m also on UHC (through my employer) and as you know, I’ve been a MDT pumper for 12ish years now. But I completely agree that this is a much bigger deal than what’s on the surface.
LikeLiked by 1 person
This gets creepier and creepier.
I LOVE your Q#3: will more patients who want/need a pump have access? It is interesting to think about the most cost effective way to give the largest number of people access to tools that allow them the best health.
Our insurance (Blue Cross RI) switched this year from covering pumps & associated supplies at 100% to covering them at 80%. So the next time we get a pump (or three–holy shit!), we will be paying a few thousand dollars. If Medtronic made it so Blue Cross would cover ITS pump at 100%, but Tandem was covered only at 80%, that would be an interesting switcheroo/mind fern. Would we be happy to have a Medtronic pump for the low price of zero dollars, or would we more happily pay 20% of the price of a Tandem pump, since it would be our choice? I don’t know.
Would a non-Medtronic pump become a status symbol?
LikeLiked by 2 people
Interesting thought about becoming a status symbol. I do tend to think, even today, there is some status associated with pumps: in some ways separating the “in-crowd” from the “old-fogey crowd”, and in other ways separating the “haves” from the “have-nots”. I’m not sure how it would turn out.
LikeLike
As always, thought-provoking post, Scott. And yes, it can make me mad. 😡
LikeLiked by 1 person
As I’ve said, you are a great writer, Scott. I love that this post brings not only the initial issue to light, but also things beyond what anyone else has said or thought.
Thank you so much for writing this.
LikeLiked by 1 person
Thanks for the post, Scott – certainly thought-provoking. Let me just pick atcha a little though.
“All pumps are, essentially, the same.” Beyond the fact that this just isn’t true except at the 50,000 foot view of the world, what else could you apply this logic to:
All meters/strips are the same.
All insulins are the same.
…
All diabetics are the same.
Back to the “All pumps are essentially the same” concept — As someone who has never used a Medtronic pump, I come to a somewhat different conclusion. Not because they aren’t a good pump and a good fit for many, many people, they are, but, because they don’t fit MY lifestyle. A Medtronic pump would not have allowed me to go sailing for 5 years, and it would not allow me to take a summer to pedal a recumbent tricycle across the US (as I am planning on doing this summer).
So the bigger question for me becomes more like, is it okay for my insurer to take a bigger step into how big/small a role diabetes plays in my life? Is it okay for my insurer to take a bigger step into the doctor/patient relationship?
I don’t know … maybe … after all, they are already there. Maybe every endo appointment should be a conference call with me, my doctor and my insurer?
LikeLiked by 2 people
Yes, this. I hate the precedent this sets, even if the thought is simple and seemingly innocent.
LikeLike
Should an insurer be forced to vary its coverage based on hobbies? If, hypothetically, a waterproof pump cost three times as much, should they cover the additional cost if the person is an avid swimmer? If so, why do I get a less-advanced pump since I don’t swim?
I’m not suggesting any particular answers, just asking the questions.
LikeLiked by 1 person
Yep, I agree that this is essentially the nub, and they are good questions.
But (again), does the alternative to NOT choosing the preferred pump/meter/strip/insulin/drug/device HAVE to be the deliberately biased appeals system where the first step on the part of the insurer is to deny your appeal? Coupled with this is when they deny your first appeal, it seems a cynical ploy to get you to just go away and accept their decision, which a significant percentage of people do. The appeal process is frequently abandoned, not because the insurer is right, but because it is too time-consuming, too frustrating, too complex and too expensive for the appellant.
Also the background is the fact that a significant premium is being paid to this company so that we might have coverage for the supplies that we need to manage a chronic illness. Why can’t we have a voice in decisions like this? Why can’t we have a voice in the range of devices and drugs?
LikeLike
For those affected, I can see your point of view. However, is this any different than insurance companies picking which meter and strips you can use? My provider (EBMS) decided that my Contour Next meter and strips were no longer covered, despite the fact that it communicates with my MDT pump/cgm. On appeal, their response was “you can manually enter your readings.” Of course. 2 years ago, they contracted with Novo-Nordisk, so Apidra insulin was no longer covered. Again, “all regular insulins are equivalent.” Heck, on a prior authorization request for a fairly new insulin product, they rejected and suggested I try Novolin or NPH (there is that Novo-Nordisk contract again). This has been going on for years, with many drugs and insurers, and is nothing new.
LikeLiked by 1 person
This goes back to question #8. It bothers me when insurers play doctor. The MDT Enlite CGM only works, on-label, with Contour Next strips. Apidra and Novolog are not the same….
LikeLiked by 1 person
Agreed, Scott. And I certain am not willing to go back 20 years to Novolin and NPH, which I why I buy my insulin choice (Afrezza) out of my own pocket. It is shameful that our insurance companies have such control. Point is, though, this is not a new problem. Just an old problem getting worse in the name of “managed care.”
LikeLike
As I wrote on Scott Strumello’s blog – call it the straw that broke the camel’s back. Also, meter/strip/insulin decisions have been largey fought at the individual level. In large part this is because (at least for me), my insurer/PBM presented those decisions as more of an individual-type decision, not a global, announce it to the world, blanket policy. Additionally, pumps are a big up-front expense. For many of us who struggle to afford the technology-based management options, it is a frightening shock to be told that your choice has suddenly been limited to a single one.
So, I think we need to wake from our slumber and realize that insurers have been interfering in the patient-doctor relationship for too long (Scott E’s point #8), while also realizing that device manufacturers have been playing a proprietary game to lock us into their ecosystems (and charge a premium to do so).
Just because it is nothing new, doesn’t mean it wasn’t wrong from the beginning.
LikeLiked by 1 person
Scott: I think it is a pure money decision nothing more or less. I believe it has to do with the CGM business and maybe some to do with the new artificial pancreas technology coming next year (I am just speculating). but I doubt we will ever know. I think our best hope is to stay together and lets others know this is an unwelcome decision.
I referred your blog to the TUDiabetes web page for the week of May 2, 2016.
LikeLike
One thing that no one has mentioned- until just recently, insurance was not mandatory. It was something most people were “lucky” to get through their employers. We, as a country took our first step towards socialized medicine with the Affordable Healthcare Act (for better or worse- the jury is still out in my mind). So now all “must” be insured. But, since when did the healthcare or insurance industries become not-for-profit? Why is UHC wrong for linking with a company they see as providing future savings via lower healthcare costs? Would any business last that does not weigh risk vs benefit? No! UHC must remain profitable for us all to remain insured.
LikeLike
And therein lies the dilemma. We can’t just ask the insurers to pay for more and more without expecting them to recoup that money somehow. But if we look to UHCs mission-statement, their own stated purpose for existence, we see that they are going astray. If you want to remove a single olive from every prepared salad, as a caterer was once known to do to save money, fine – that’s entirely a business decision. But when you directly impact the health of your customers, there are other factors that should go into these decisions.
LikeLike
I don’t think all pumps are pretty much the same though. For my super active 5 year old, being tubeless is a big deal and MDI can’t deliver the small increments he needs. I don’t mind paying the difference in cost for a pump preference, but it doesn’t sound like that will be the new model. It’ll be Medtronic or nothing. Not an allowance where you can have a Medtronic covered at s higher rate or a preferred pump at a lower rate.
LikeLike
My understanding is that, under the specifics of this arrangement, Omnipod isn’t (and hasn’t been) considered DME by UHC so it is unaffected.
LikeLike
Lots to think about here. It does make me concerned that my daughter will someday feel stuck using a product that isn’t at all her choice. She is covered under UHC and using MDT, and were switching in a few months, but now not. All in all, this leaves me feeling like we have little control. Thanks to binge-watching Downton Abbey, I’m spending these recent days considering our luck in living in a time where insulin and a device to deliver it are at our fingertips. I hope it sticks.
LikeLike
Pingback: Friday Five: WTF Happened This Week? – See Jen Dance
Pingback: Here’s my damn (#DiabetesAccessMatters NOW) story | Rolling in the D
Pingback: What TuDiabetes members are saying about UHC/Medtronic decision - Diabetes Hands Foundation